Why Image Processing?
Currently, a clinical diagnosis for Glaucoma detection is performed under the supervision of a trained ophthalmologist. There is no such tool designed yet which can give a decision in absence of medical expert. So, an automated diagnostic tool can be used for screening purpose at primary care centres. Such a tool can act as an assisting tool and screen the affected patients so that proper medical care can be provided to them.
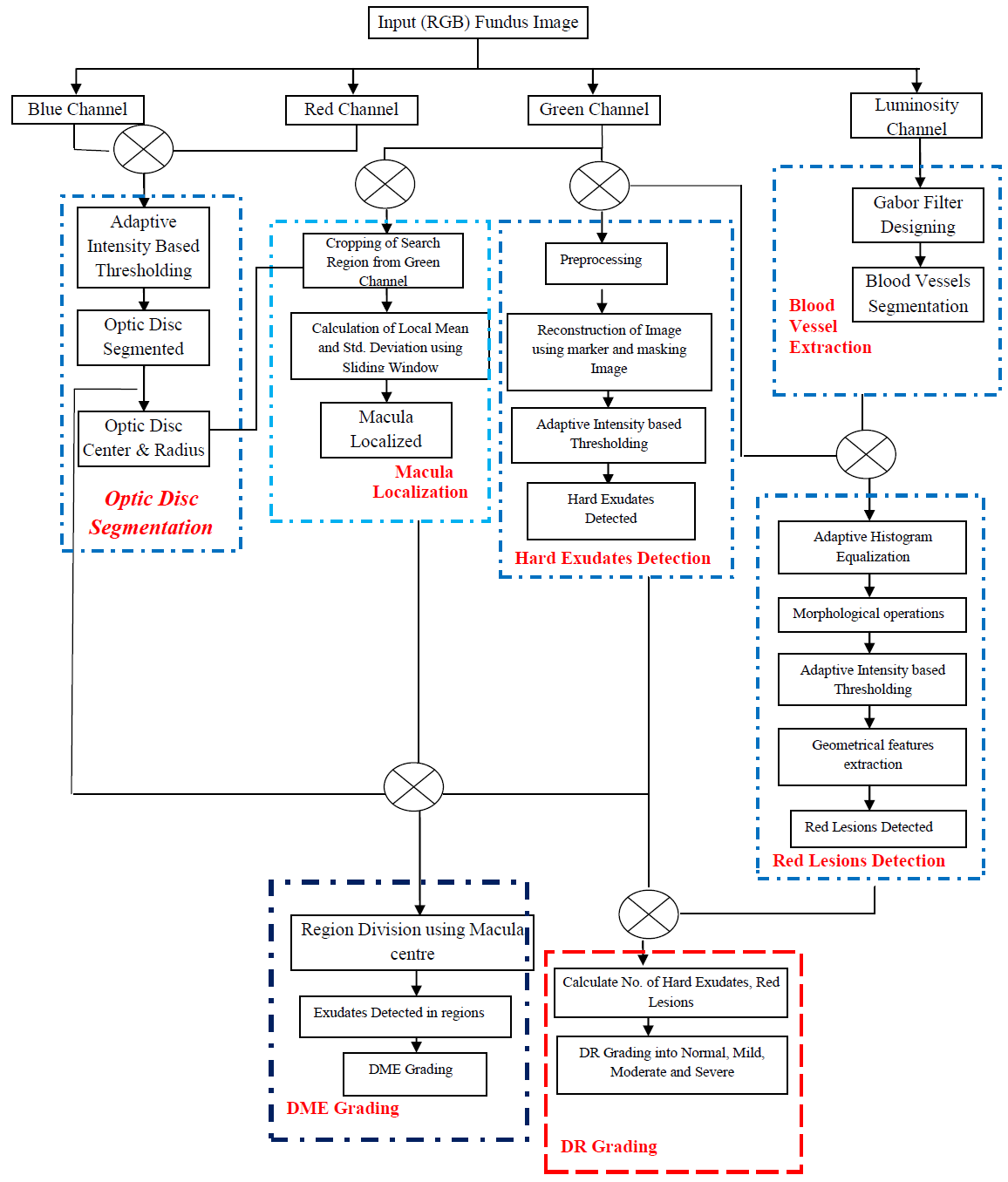
The medical signs such as cupping of optic disc, haemorrhages, blood vessel abnormality, peri-papillary atrophy and RNFL defects are some clinical observations used by medical experts across the globe. These clinical observations impart visual changes to a fundus image and can easily be differentiated from an image which has no signs.
Visual changes like change in intensity and colour of pixels, tortuosity of blood vessels can be observed which can be easily detected using IMAGE PROCESSING techniques. Also, the diagnosis is done by considering the clinical input from medical experts, so there are less chances of wrong diagnosis.

Challenges
Glaucoma is a disease majorly related to the optic nerve head region. Structural changes may occur in the optic nerve head region which may characterize the presence of Glaucoma. Since, the disease is related to optic nerve head region, so this region should be segmented accurately using image processing techniques. However, the presence of medical signs like bright lesions (exudates and cotton soft wools) and some artefacts which gets introduced in the images during acquisition process, affect the accuracy of optic disc segmentation. The following can be considered some important challenges which are faced during ONH segmentation:
- Exudates
- Reflections (artefacts introduced due to illumination)
- Correct ONH localization
- Choroid Vessels
- Blood Vessels overlaying on the ONH region